Protecting Your Smile: My Guide to Preventing Dental Problems After Gastric Bypass
Introduction: The Unexpected Link Between Gastric Bypass and Oral Health
When I decided to have gastric bypass surgery, I thought I knew what was coming. I prepared myself for lifestyle changes—new eating habits, vitamin pills, and even times when the weight loss stopped. What surprised me, though, was how quickly the surgery affected my teeth and gums.
If you’re like me, you probably had the same goal: get healthy, lose weight, and improve your life. Nobody told me dental problems would show up out of nowhere. Suddenly, I started noticing sensitive teeth, more cavities, and a dry mouth I just couldn’t get rid of. That’s when I realized I needed a whole new way to take care of my mouth.
I want to share what I’ve learned the hard way, so you don’t have to go through the same surprises. In this guide, I’ll explain why gastric bypass impacts your mouth, what problems to look out for, and, most importantly, what you can do to keep your smile healthy and confident for years to come.
Table of Contents
Why Gastric Bypass Impacts Oral Health: Understanding the Reasons
You might wonder why a surgery on your stomach has anything to do with your teeth. I didn’t get it at first, either. But after a few long talks with my dentist and some trial-and-error, I realized several changes after surgery can mess with your mouth.
Increased Acid Exposure
One bad surprise for many people after bypass surgery is acid reflux (GERD). I started waking up with a sour taste in my mouth and, sometimes, a burning throat. But more than being uncomfortable, acid can wear away tooth enamel—a shield you can’t grow back once it’s gone.
Some patients also struggle with feeling sick and throwing up, especially in the first year. Each time stomach acid comes up, it covers your teeth in strong acid. And the damage can build up.
Key point? Even if you never had reflux before, watch out for new symptoms after gastric bypass.
Dry Mouth (Xerostomia)
At first, I didn’t think much of always being thirsty. It turned out to be dry mouth, or xerostomia, which is way more than just “cotton mouth.” Gastric bypass makes this common because you might not have enough water in your body or from medicines you take after surgery.
Why does this matter? Saliva is like your mouth’s cleaning crew. It balances out acid and helps wash away bacteria and food bits. When there’s less of it, your risk for cavities and infections goes way up. I found myself needing water by my side all day—and still feeling very thirsty.
Lack of Nutrients and Poor Absorption
Bariatric surgery, especially gastric bypass, changes how your body takes in vitamins and minerals from food. Think of it like a filter—everything you eat has to get through a smaller gate.
Here are a few nutrients that gave me trouble:
- Calcium and Vitamin D: Low levels mean your teeth and jawbone get weaker over time.
- Vitamin B12, Iron, Folate: Not enough can cause mouth sores, gum infections, and problems with healing.
- Protein: Your body needs it to fix tissues—including those in your mouth.
Even though I took my supplements every single day, my blood tests sometimes told a different story. It’s not always what you’re taking, but what your body is actually using.
Dietary Changes and Snacking Habits
After gastric bypass, I switched to eating small, frequent meals. I also noticed I often chose softer, sometimes sweeter foods, because tougher foods felt heavy and caused discomfort.
The problem is, snacking all the time gives bacteria in your mouth plenty of food (especially from sugars and starches). They start to party, making acids that break down your teeth bit by bit. Acidic drinks and foods—like citrus and juice—don’t help the situation, either.
I learned the hard way that snacking all day, even on healthy foods, can be hard on your enamel.
Common Dental Problems After Gastric Bypass
Once I learned how surgery made the problems possible, the issues I started to see made more sense. Here’s what to look for.
Dental Erosion
A dentist explained it like this: every time acid touches my teeth, it removes a tiny layer of enamel. Over time, that protective layer gets thinner. My teeth started feeling and looking different—more yellow, a little oddly shaped, and sensitive to anything cold.
About half of bariatric patients see moderate to severe erosion at some point, especially near the gumline.
Tooth Decay and Cavities
Tooth decay is bad enough on its own, but after gastric bypass, the risk doubles or even triples. I suddenly found myself facing more cavities than ever. Sugar is an obvious cause, but sticky or soft foods (even “healthy” ones) can stick around your mouth and cause decay.
Cervical (gumline) and root cavities are especially common post-surgery, since that’s where mouth fluids and food bits tend to stick around. I had to get serious about flossing and getting a better toothpaste.
Gum Disease (Gingivitis & Periodontitis)
Swelling and infection of the gums can start fast—especially if you’re low on nutrients or struggling with cleaning your mouth. Bleeding, puffiness, and even gums pulling back showed up for me within a year. My dentist told me gum disease can get worse quickly and lead to tooth loss if you ignore it.
Tooth Sensitivity
I couldn’t enjoy an ice-cold drink without cringing. That’s because when enamel wears away or gums pull back, nerves in your teeth are uncovered. I found that even brushing my teeth sometimes hurt.
Using the right toothpaste and being gentle with my brushing way helped a lot.
Oral Thrush and Angular Cheilitis
After surgery, I dealt with a couple of yeast infections inside my mouth (oral thrush) and painful cracks at the corners of my lips (angular cheilitis). Both were caused by dry mouth, a weaker immune system, and not getting enough nutrients. These conditions are uncomfortable and keep coming back if you don’t fix the main problem.
Steps I Take to Protect My Teeth and Gums
All these issues sound scary, but here’s the good news: you can do a lot to help. Here’s what has worked for me (and what many experts now recommend).
Improving My Teeth Cleaning Routine
I had to do a better job when it came to oral care. Here’s what changed:
- Brushing Twice a Day (Gentle, but Complete): I switched to a soft-bristled toothbrush and fluoride toothpaste (sometimes even a stronger kind from a doctor). I brush after breakfast and before bed, being careful not to scrub too hard.
- Daily Flossing: Skipping this step isn’t an option anymore. I use floss or sometimes tiny brushes for between teeth. It’s the only way to get all the food bits out from between my teeth.
- Special Mouthwash: Alcohol-free, fluoride, and sometimes a pH-balancing kind. My mouth feels clean, but not dried out.
- Electric Toothbrush: This has made a huge difference in getting rid of plaque, especially when I’m tired or in a hurry.
If you want to learn more about the basics of dental care, there are some good guides out there covering the basics and advanced tips.
Changing How and What I Eat
Changing what, when, and how I eat helped my teeth a lot:
- Limit Sugar and Acid: I had less diet sodas, citrus, fruit juices, and chewy candies. Even “healthy” smoothies caused issues when drinking them all day.
- Rinse After Eating or Throwing Up: I keep a small bottle of water (or a water mixed with baking soda) on hand and rinse after snacks and meals.
- Chew Xylitol Gum (Sugar-Free): This not only fights bacteria but helps make more spit. My dentist recommended it for dry mouth.
- Drink Plenty of Water: I sip water all day, but I try not to sip on drinks all day—otherwise, my teeth are always exposed to whatever is in the liquid.
- Avoid Snacking All the Time: It’s hard, but I aim for set meal times rather than mindless snacking. Less exposure means less risk for decay.
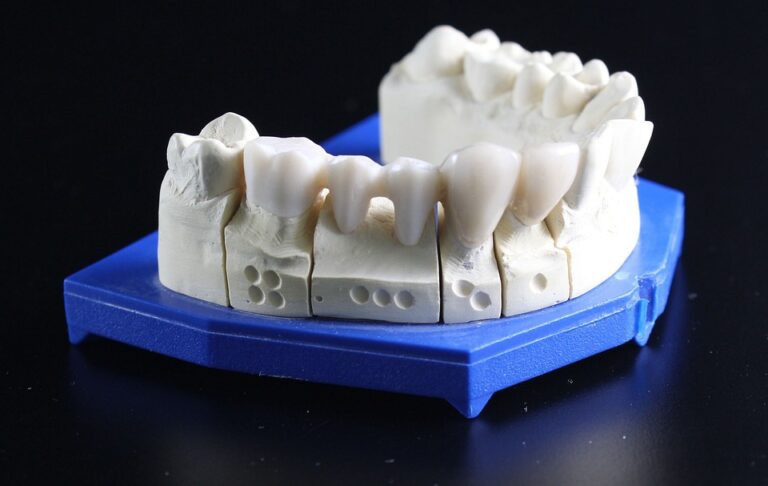
When I need deeper cleaning because of tough stains or buildup, seeing a dental ceramics lab for professional help is often worth it.
Handling Special Problems After Surgery
Some solutions were new to me, but they’ve helped a lot:
- Dry Mouth: I use products from the store that help you make more spit, occasionally fake spit (not the tastiest, but it works), and I run a machine that adds moisture to the air at night.
- Acid Reflux/GERD: Medication (from my doctor), sleeping with my head slightly raised, and avoiding foods that cause problems before bed reduced my reflux episodes.
If acid damage keeps returning, a night guard dental lab may be helpful. A custom night guard can protect your teeth from acid when you can’t control reflux while sleeping.
Making Sure I Get Enough Nutrients
Supplements are a must after gastric bypass. I stick to my plan on schedule:
- Calcium and Vitamin D: I take them every day, in smaller amounts at different times for better absorption, plus my bariatric multivitamin.
- B12, Iron, Folate: My surgeon checks my bloodwork every few months, and I change the amount as needed.
- Protein: I aim for lean protein at every meal—think eggs, fish, chicken, yogurt.
When I felt overwhelmed, working with a food expert gave me a plan I could actually follow—and my dentist noticed the difference in my mouth health at my next check-up.
Seeing the Dentist Regularly
Here’s where working together helps. I’m honest with my dentist about my gastric bypass so they can personalize my care:
- Frequent Check-Ups: I go every three to six months, at least for the first few years.
- Professional Cleanings: These remove stubborn plaque and tartar I just can’t get at home.
- Preventive Treatments: My dentist applies fluoride varnish every few visits and sometimes uses sealants for back teeth that might get cavities.
- Tell Them Everything: I mention any new symptoms, even if I think they’re small.
If you’re interested in fixing teeth—whether that’s crowns or bridges—a crown and bridge lab or veneer lab offers options. Just remember, it’s easier to prevent problems than to fix them!
When I Know It’s Time to Call My Dentist
I’ve learned not to wait when certain symptoms pop up. If you’re not sure, here’s my general rule:
- Long-lasting Sensitivity or Pain: If a tooth keeps hurting, don’t ignore it.
- Visible Changes: New pits, yellow spots, or thinning enamel often mean erosion or decay.
- Bleeding or Swollen Gums: Ignoring this lets gum disease get started.
- Bad Breath That Won’t Go Away: This can be a sign of dry mouth or infection.
- Mouth Sores, Thrush, or Cracking Lips: These might be a sign of bigger nutrition problems.
Catching these problems early has saved me more trouble (and money) than I can count.
Conclusion: Keeping My Smile Healthy for Good
Having gastric bypass surgery changed everything for me—my body, my relationship with food, and, unexpectedly, my oral health. It’s not always easy. But by knowing what to do, getting help, and not giving up, you can avoid most dental problems that come with weight loss surgery.
Remember: stick with your oral hygiene, keep up your nutrition, and work closely with your dentist and bariatric team. Don’t let dental issues ruin the happiness from your weight loss success.
Believe me, you’ll be glad you did it later.
References & Further Reading
- Dental Diseases and Conditions
- Teeth and Overall Health
- Dental Care and Aesthetics
- Teeth Information & FAQ
- Bariatric Surgical Practice and Patient Care (2016)
- Obesity Surgery (2017)
- Journal of Oral Maxillofacial Surgery (2014)
- Clinical Oral Investigations (2018)
- Journal of Dental Research (2020)
- Additional academic and clinic-based recommendations from bariatric dental experts
Have your own questions or experiences about dental care after gastric bypass? Don’t hesitate to reach out to your healthcare team—and take action today for your smile.