Does Suboxone Cause Dental Problems? Understanding Risks & Protecting Your Oral Health
By someone who’s been there, learned a lot, and wants you to keep your smile strong.
Introduction
When I first heard about Suboxone, it sounded like hope in a tiny orange film—a lifesaver for folks, including me, struggling with Opioid Use Disorder (OUD). No doubt, Medication-Assisted Treatment (MAT) with Suboxone (a mix of buprenorphine and naloxone) can turn your life around. But as my recovery went on, another problem started bugging me: what’s happening to my teeth?
I noticed more cavities, sore teeth, and honestly felt like my mouth was getting worse. At first, I just ignored it, thinking this was just bad luck or from past neglect. But then I saw post after post online, news stories, and even lawsuits, all asking the same thing: Does Suboxone cause dental problems?
I went deep into the subject—reading articles, asking my dentist, talking with others, and trying everything suggested for oral health. In this article, I want to share what I found: how Suboxone really affects your teeth and gums, why it happens, what else plays a part, and—most importantly—what you can do to keep your smile safe while you stay on your recovery path.
Table of Contents
- How Suboxone Impacts Your Teeth and Gums
- Beyond Suboxone: Contributing Risk Factors
- Protecting Your Smile: Prevention and Management Strategies
- Awareness, Lawsuits, and Patient Advocacy
- Conclusion
How Suboxone Impacts Your Teeth and Gums
Understanding the Ways Damage Happens
First, let’s clear up a mistake many people make: it’s not the Suboxone itself that directly chews up your teeth (even though it kind of feels that way). The problem is really about how the medicine is made, how it works, and the way you use it.
#### High Acidity (Low pH) – The “Quiet Eroder”
Remember a little from science class? Suboxone films and tablets—especially the ones you put under your tongue or by your cheek—are acidic. Over time, this low pH can wear down the hard, shiny layer on your teeth called enamel. It’s like holding a lemon slice against your tooth for hours, every day.
I used to think, “I let the film dissolve, then I’m done.” But nope—the acid hangs around, making it easy for bad bugs to have a party in your mouth.
#### Dry Mouth (Xerostomia) – The “Hidden Problem”
The second big cause is dry mouth (what dentists call xerostomia). Buprenorphine, one of the main ingredients in Suboxone, tends to make your mouth drier. Saliva is your mouth’s best friend—it rinses out food, keeps acids in check, and fights off cavities. Without enough spit, cavities pop up quicker, your gums get sore, and your mouth feels dry and sticky.
#### How You Take Suboxone – Where and How Makes a Difference
Think about how long those Suboxone films or tablets sit against your gums and teeth. They stay there as they dissolve, leaving those areas in touch with acidity longer. Sometimes the spot where I held the film would get sore or even turn white—an early warning my mouth didn’t like what was going on.
Dental Problems People See with Suboxone
After about a year on Suboxone, my dentist looked worried. “Have you been eating lots of sugar?” he asked. But I wasn’t—the cavities seemed to show up out of nowhere. And I’m not the only one.
Here are the main dental issues I—and lots of others—have gone through:
- Bad & Fast-Moving Cavities: Not just tiny spots. Sometimes several teeth, getting worse quickly.
- Enamel Wear: That strong, shiny outside of your teeth gets thin, making teeth feel weak and sensitive. When enamel is gone, it won’t grow back.
- Gum Disease (Gingivitis & Worse): Dry mouth messes up the normal bacteria mix. Gums turn red, swell up, bleed, or even get infected.
- Tooth Sensitivity and Pain: Eating ice cream or even a cold breeze can really hurt.
- Teeth Breaking or Falling Out: Weakened teeth snap and break more often—sometimes down to tiny pieces.
- Mouth Infections (like thrush or ulcers): Less spit makes it easier for yeast and germs to grow.
- Bad Breath: Not fun, but also a sign something’s wrong.
For many, these problems are way more than “just a side effect.” Sometimes it means thousands in dentist bills—or losing teeth for good.
Beyond Suboxone: Contributing Risk Factors
Blaming only Suboxone would be missing the point (and a bit unfair). In my experience, lots of other things played a part, too. Think of dental problems as a group project—Suboxone might be the leader, but other things join in.
Already Bad Oral Health
Many of us who used opioids before weren’t starting recovery with perfect teeth. Years without dentist visits, not brushing much, or brushing badly meant I already had some cavities and maybe bad gums.
Plus, being scared of going to the dentist made things worse, especially early in recovery. If you already had a hard time taking care of your mouth or even seeing a dentist, starting Suboxone can push those problems over the edge.
Lifestyle and Eating Habits
Your habits play a huge role. Let’s be real here:
- Not brushing or flossing enough (or correctly): Sometimes it’s hard to keep up, even if you want to.
- Eating and drinking sugary or sour stuff: Juice, soda, candy—these help bad bacteria, and the Suboxone acid doesn’t help things.
- Smoking or chewing tobacco: Makes your mouth even drier.
- Skipping dentist appointments: I found out the hard way that skipping cleanings is like never changing your oil in your car. It works for a while… until it doesn’t.
How Long and How Much Suboxone You Use
I started noticing my teeth’s problems after about nine months of taking Suboxone every day. Studies say the longer you’re on it, and the more you take, the higher the risk. For some people, just a few months is enough—especially if they already had weak teeth.
Protecting Your Smile: Prevention and Management Strategies
Once I knew what was happening, I started looking for fixes. Here’s what really helped me—and what dentists say works best:
Boost Your Brushing and Flossing
If you only do one thing, do this: really good brushing and flossing saves your teeth.
- Brush twice a day with fluoride toothpaste. Don’t rush—use a timer if you want.
- Floss once daily. Even if it feels like too much, it pays off.
- Pick an alcohol-free mouthwash with fluoride. Alcohol dries your mouth more, which you don’t want.
- Rinse your mouth out right after you take your Suboxone. Wash away leftover acid fast before it does any harm.
I made these steps my daily routine—sometimes even sticking reminders on my mirror. It wasn’t easy at first, but it made a huge difference. At my six month check-up, for the first time in a while, I had no new cavities.
Tackling Dry Mouth (Xerostomia)
A dry mouth just gets worse if you ignore it. Here’s what I found useful:
- Sip water often. Keep a water bottle nearby and drink before and after your dose.
- Chew sugar-free gum or suck on sugar-free candies. This helps your mouth make more saliva.
- Try saliva sprays or gels from the pharmacy. Sometimes a doctor can give you something stronger if you need.
- Stay away from caffeine, booze, and sugary drinks. They make dry mouth worse.
When I didn’t deal with dry mouth, my cavities showed up even faster. When I did take care of it, things slowed down a lot.
Eating Smarter
I stopped drinking soda and mostly had water. Sweet stuff became just an occasional treat. Foods like cheese, plain yogurt, and raw veggies help—they protect your teeth and help your mouth make more spit.
I was shocked at how much those simple swaps mattered. Candy used to seem harmless, but on Suboxone, even a little could wreck my teeth.
Keep Up with Dental Visits
Honestly, going to the dentist with a lot of cavities was tough. But you have to do it. Here’s what helped me, and what every Suboxone user should think about:
- Go in for a cleaning and check-up every 3-6 months. Don’t wait for pain—catch problems early.
- Tell your dentist you’re taking Suboxone. They need to know—trust me, it’s not the first time they’ve heard it.
- Ask about extra protection. Things like fluoride gel, sealants, or stronger toothpaste can help keep your teeth tough.
- Speak up if you’re nervous. A good dentist will help you feel better, not judge you.
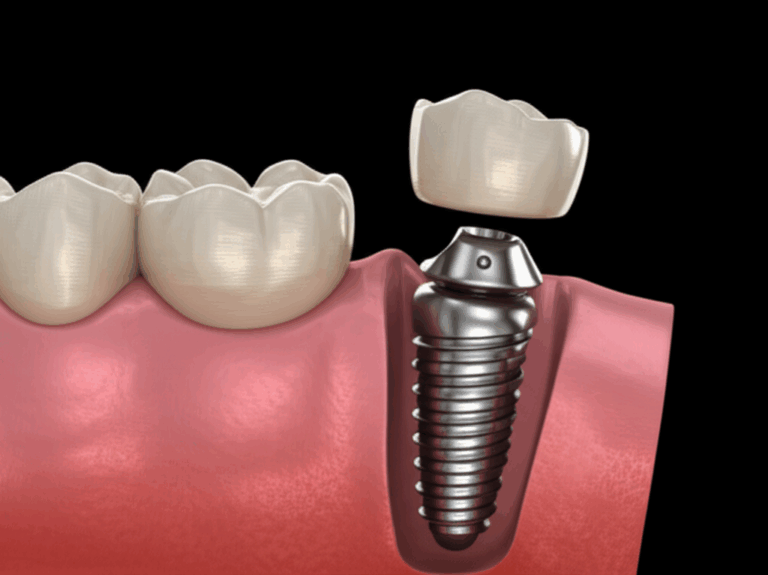
If you want info on fixing big dental problems—like crowns, implants, or dentures—labs like crown and bridge lab or implant dental laboratory are options your dentist can talk about.
Talk to Your Doctors
At my check-up, I told my doctor about my teeth. She explained how Suboxone affects them and gave me advice. For some people, there are other ways to get buprenorphine, like a shot, so it doesn’t mess with your mouth. If that might be something for you, ask your prescriber—but don’t stop treatment yourself.
Managing pain after getting dental work is also different when you’re on MAT. Make sure your dentist, oral surgeon, and addiction doctor know what you’re taking so they can help you safely.
Awareness, Lawsuits, and Patient Advocacy
By 2023, the news was full of stories about people suing Suboxone makers for not warning them about the tooth risks. Suddenly, dentists, drug companies, lawmakers—all started paying attention.
The FDA now says Suboxone must have a warning about tooth troubles. That doesn’t fix your teeth fast, but it does mean new people should know what might happen, and get more advice on keeping teeth safe.
If you think your dental problems are from Suboxone and want to know your rights, you can get in touch with advocacy groups or legal helpers. In my experience, though, early action is always better—and making sure your dentist and doctor talk to each other.
Conclusion
Thinking back, would I trade my recovery for perfect teeth? No way. But I wish I knew before what Suboxone could do to your mouth, and had a plan to protect my teeth sooner.
For me, the link between Suboxone and tooth trouble is real—but it’s not automatic. It’s about knowing what could happen, taking care of your teeth right, making smart food choices, and being open with your doctors.
Don’t let being scared or embarrassed stop you: look after your teeth just like you look after your recovery. Your smile is part of who you are—it deserves care too.
If you want more favorites on mouth health, check out these easy guides on teeth health and dental care.
Remember: your recovery means the world. But your teeth matter as well—and you can look after them both.
This article is based on my own story and the lessons I had to learn the hard way. If you’re in the same situation, don’t let embarrassment or confusion slow you down. Reach out to your dentist, doctor, or support group for help. You’ve got this.